Research Highlights:
- Incorporating remote blood pressure monitoring into post-stroke care was found to be feasible and beneficial for stroke survivors who live in a historically under-resourced community.
- A new telehealth care strategy for stroke survivors improved patient engagement, patient access and blood pressure levels three months after the first stroke.
Embargoed until 4 a.m. CT/5 a.m. ET Thursday, Feb. 3, 2022
 (NewMediaWire) – February 03, 2022 – NEW ORLEANS – A new strategy using telehealth to monitor blood pressure at home for several months immediately after a stroke had a positive impact on patient engagement and blood pressure control among people who live in historically under-resourced communities, according to preliminary research to be presented at the American Stroke Association’s International Stroke Conference 2022, a world premier meeting for researchers and clinicians dedicated to the science of stroke and brain health to be held in person in New Orleans, and virtually, Feb. 8-11, 2022.
(NewMediaWire) – February 03, 2022 – NEW ORLEANS – A new strategy using telehealth to monitor blood pressure at home for several months immediately after a stroke had a positive impact on patient engagement and blood pressure control among people who live in historically under-resourced communities, according to preliminary research to be presented at the American Stroke Association’s International Stroke Conference 2022, a world premier meeting for researchers and clinicians dedicated to the science of stroke and brain health to be held in person in New Orleans, and virtually, Feb. 8-11, 2022.
Having an ischemic stroke (caused by a blocked blood vessel leading to the brain) greatly increases the risk of having another stroke. It’s important to prevent a second stroke because the chance of serious disability increases significantly with every additional stroke.
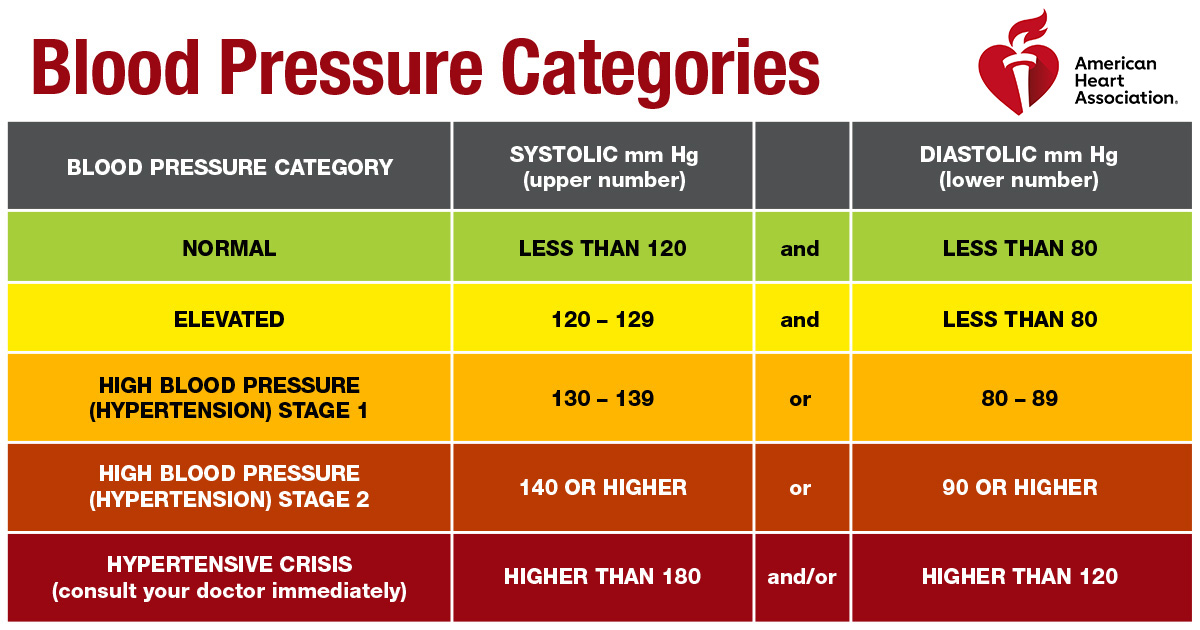
“Hypertension is the most important modifiable risk factor for a second or recurrent stroke. We know that a small change to lower systolic blood pressure [the top number in a blood pressure reading] reduces recurrent stroke risk by more than 20%. Yet, blood pressure is poorly controlled among more than half of stroke survivors,” said Imama A. Naqvi, M.D., lead study author, an assistant professor of neurology at Columbia University Vagelos College of Physicians and Surgeons, and a neurologist with New York-Presbyterian/Columbia University Irving Medical Center, both in New York City. “We also know that Black adults have a higher prevalence of uncontrolled blood pressure. In addition, Black and Hispanic populations have a higher risk of stroke, and the highest increase in stroke prevalence is expected to be among Hispanic males.”
In this feasibility study, the researchers from Columbia University tested the potential impact of a new, multi-disciplinary strategy called Telehealth After Stroke Care (TASC) for stroke survivors who received post-stroke care at NewYork-Presbyterian/Columbia University Irving Medical Center. The study took place in the Northern Manhattan area, with an underserved community. Participants included 50 stroke survivors (44% were Hispanic adults; 32% Black adults; and 20% white adults), with an average age of 64. About half (54%) of the participants had up to a high school education, and 30% had private health insurance. They were randomly divided into two groups: half of the study participants received usual care (the control group); the other half of the study participants were supported with enhanced telehealth after their stroke (the intervention group). Both groups were enrolled before hospital discharge and followed for 90 days, the window of time when the risk of having another stroke is the highest.
Patients assigned to the control group had a video conference appointment with a primary care professional one to two weeks after hospital discharge, and video conference appointments with a stroke specialist at 6 and 12 weeks after discharge. Participants in the enhanced telehealth group received mobile tablet devices, blood pressure monitors and video visits with a multidisciplinary team including pharmacy support. The home blood pressure monitor remotely sent the participant’s readings to the patient’s electronic health record. Based on these remote readings, a nurse provided call support and could escalate to telepharmacists and physicians, if needed. The enhanced telehealth group also received a plain-language blood pressure infographic in English or Spanish, specifically tailored to their individual health information, to help educate them about healthy blood pressure levels, goals and ways to improve their blood pressure. Home blood pressure was measured at the end of the study.
Key findings from the study included:
- The Telehealth After Stroke Care strategy had a significant improvement in patient follow-up: 84% of patients in the enhanced telehealth group completed the 12-week study, compared to 64% of patients in the usual care group.
- 91% of patients in the enhanced telehealth group completed the video visit with primary care professionals and specialists, compared to 75% of patients in the usual care group.
- Blood pressure control was better in the enhanced telehealth group at 76%, compared to 25% control in the control group.
- Among Black study participants, blood pressure control improved from 40% of participants at enrollment to 100% at the study’s conclusion in the enhanced telehealth group and improved only from 14% to 29% in the control group.
“COVID-19 has highlighted numerous health inequities that make post-stroke care more difficult and created a gap in health outcomes for people from diverse racial and ethnic groups. We need to devise ways to bridge this divide,” said Naqvi. “Mobile health tools such as wireless blood pressure devices that enable remote monitoring are here to stay, and we need to find ways to utilize telemedicine to improve care for all stroke survivors. As physicians, we want to provide patients with equitable access to care and find the right post-stroke care interventions that engage patients and improve health outcomes.”
Researchers urge caution regarding interpreting results from this feasibility study; while promising, these findings warrant further replication in a larger trial.
“This new research will continue to strengthen our work and commitment to addressing health inequities, by focusing on blood pressure through regular remote monitoring and partnering with our patients,” said Willie Lawrence, M.D. , chairman of the American Heart Association’s National Hypertension Control Initiative’s oversight committee. “The goal of the National Hypertension Control Initiative is to improve blood pressure control rates in historically under resourced communities. By applying a multi-faceted approach that includes comprehensive training and technical assistance for professionals in community health centers, collaboration with trusted community-based organizations and direct patient education, we hope to empower communities with blood pressure education and resources that can improve outcomes before a stroke occurs but also create a network of care and support after a stroke.”
Study co-authors are Kevin H. Strobino, M.P.H.; Kevin Schmitt, M.S.; Jessica Li; Hanlin Li, Pharm.D., M.B.A.; Marie Garcon, N.P.; Sarah Tom, Ph.D., M.P.H.; Adriana Arcia, Ph.D., R.N.; Olajide A. Williams, M.D., M.S.; Ken Cheung, Ph.D.; Ian M. Kronish, M.D., M.P.H.; and Mitchell S. Elkind, M.D., M.S. The list of authors’ disclosures is available in the abstract.
Statements and conclusions of studies that are presented at the American Stroke Association and American Heart Association’s scientific meetings are solely those of the study authors and do not necessarily reflect the Association’s policy or position. The Association makes no representation or guarantee as to their accuracy or reliability. Abstracts presented at the Association’s scientific meetings are not peer-reviewed, rather, they are curated by independent review panels and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting. The findings are considered preliminary until published as a full manuscript in a peer-reviewed scientific journal.
The Association receives funding primarily from individuals; foundations and corporations (including pharmaceutical, device manufacturers and other companies) also make donations and fund specific Association programs and events. The Association has strict policies to prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers and health insurance providers and the Association’s overall financial information are available here.
Additional Resources:
The American Stroke Association’s International Stroke Conference (ISC) is the world’s premier meeting dedicated to the science and treatment of cerebrovascular disease. ISC 2022 will be held in person in New Orleans and virtually, Feb. 8-11, 2022. The three-day conference will feature more than 1,500 compelling presentations in 17 categories that emphasize basic, clinical and translational sciences as research evolves toward a better understanding of stroke pathophysiology with the goal of developing more effective therapies. Engage in the International Stroke Conference on social media via #ISC22.
About the American Stroke Association
The American Stroke Association is devoted to saving people from stroke — the No. 2 cause of death in the world and a leading cause of serious disability. We team with millions of volunteers to fund innovative research, fight for stronger public health policies and provide lifesaving tools and information to prevent and treat stroke. The Dallas-based association officially launched in 1998 as a division of the American Heart Association. Connect with us on stroke.org, Facebook, Twitter or by calling 1-888-4STROKE.
###
For Media Inquiries and AHA Expert Perspective:
AHA Communications & Media Relations in Dallas: 214-706-1173; ahacommunications@heart.org
Karen Astle: 214-706-1392; karen.astle@heart.org
For Public Inquiries: 1-800-AHA-USA1 (242-8721)
heart.org and stroke.org